Wii_Hab
- Dettagli
- Visite: 3620
Video Installazione Software Wii_Hab in Italiano
Il software si puo scaricare a questo indirizzo:
http://www.osteomedicina.it/index.php/wii-hab/category/9-wii-hab-italiano
Video Installazione Software Wii_Hab in Italiano
Il software si puo scaricare a questo indirizzo:
http://www.osteomedicina.it/index.php/wii-hab/category/9-wii-hab-italiano
1Department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine
Pneumonia is one of the top ten leading causes of death in the U.S. Osteopathic manipulative techniques (OMT) may be utilized as an adjunctive therapy in the treatment of pneumonia to enhance biomechanical and immune function; and ultimately, to reduce hospital stay, duration of antibiotics, incidence of respiratory failure, and mortality. In this video-article, we will review randomized controlled studies on the use of OMT in pneumonia patients, as well as demonstrate specific hands-on techniques that are routinely practiced by osteopathic physicians when treating pulmonary infections.
Date Published: 5/06/2014, Issue 87; doi: 10.3791/50687
Keywords: Medicine, Issue 87, Pneumonia, osteopathic manipulative medicine (OMM) and techniques (OMT), lymphatic, rib raising, thoracic pump, muscle energy, doming diaphragm, alternative treatment
Cite this article
Yao, S., Hassani, J., Gagne, M., George, G., Gilliar, W. Osteopathic Manipulative Treatment as a Useful Adjunctive Tool for Pneumonia. J. Vis. Exp. (87), e50687, doi:10.3791/50687 (2014).
Pneumonia, the inflammatory state of lung tissue primarily due to microbial infection, claimed 52,306 lives in the United States in 20071 and resulted in the hospitalization of 1.1 million patients2. With an average length of in-patient hospital stay of five days2, pneumonia and influenza comprise significant financial burden costing the United States $40.2 billion in 20053. Under the current Infectious Disease Society of America/American Thoracic Society guidelines, standard-of-care recommendations include the rapid administration of an appropriate antibiotic regiment, fluid replacement, and ventilation (if necessary). Non-standard therapies include the use of corticosteroids and statins; however, these therapies lack conclusive supporting evidence4. (Figure 1)
Osteopathic Manipulative Treatment (OMT) is a cost-effective adjunctive treatment of pneumonia that has been shown to reduce patients’ length of hospital stay, duration of intravenous antibiotics, and incidence of respiratory failure or death when compared to subjects who received conventional care alone5. The use of manual manipulation techniques for pneumonia was first recorded as early as the Spanish influenza pandemic of 1918, when patients treated with standard medical care had an estimated mortality rate of 33%, compared to a 10% mortality rate in patients treated by osteopathic physicians6. When applied to the management of pneumonia, manual manipulation techniques bolster lymphatic flow, respiratory function, and immunological defense by targeting anatomical structures involved in the these systems7,8, 9, 10.
The objective of this review video-article is three-fold: a) summarize the findings of randomized controlled studies on the efficacy of OMT in adult patients with diagnosed pneumonia, b) demonstrate established protocols utilized by osteopathic physicians treating pneumonia, c) elucidate the physiological mechanisms behind manual manipulation of the respiratory and lymphatic systems. Specifically, we will discuss and demonstrate four routine techniques that address autonomics, lymph drainage, and rib cage mobility: 1) Rib Raising, 2) Thoracic Pump, 3) Doming of the Thoracic Diaphragm, and 4) Muscle Energy for Rib 1.5,11
Children, elderly individuals, and immunocompromised patients are especially susceptible to pneumonia. Patients may present with fever, cough, dyspnea, tachypnea, tachycardia, sputum production, pleuritic chest pain, nausea, vomiting, diarrhea, and fatigue4. Clinical chest examination may reveal dullness to percussion and crackles upon auscultation over the affected lung12. Laboratory results may show a leukocytosis with left-shift, as well as an increase in erythrocyte sedimentation rate and C-reactive protein4. Tests to elucidate the specific causative microbe include the urine antigen test, polymerase chain reaction, sputum analysis, and blood culture4. Finally, radiographic imaging, which serves as the gold standard for diagnosis, may display consolidation or inflammatory changes over the various lobes of the lungs12. While no specific algorithm or constellation of symptoms have consistently proven to establish the clinical diagnosis of pneumonia, temperature > 100º F and abnormal breath sounds (rales or rhonchi) are generally accepted as criteria for ordering a chest x-ray or sputum sample13. Additionally, the Pneumonia Severity Index (PSI) and CURB-65 criteria have been proven to accurately predict mortality in pneumonia patients.14, 15
Once the diagnosis of pneumonia has been confirmed, traditional standard-of-care management should be administered. For patients in a stable condition, osteopathic evaluation and adjunctive treatment may be beneficial and should be considered.
In addition to being fully-licensed to practice conventional medicine, osteopathic physicians utilize a multi-step holistic approach to diagnosis and treatment that improves structure, function, and the body's intrinsic ability to heal. Management begins with taking a standard history and performing a physical exam. If necessary, laboratory and imaging studies are conducted. An osteopathic structural exam is then performed, which includes an evaluation and assessment of the following parameters which are beyond the scope of this article: presence of segmental and regional restrictions of motion, thoracic cage immobility, muscle spasms, tenderpoints, viscerosomatic reflexes, Chapman's points, lymphatic obstructions, autonomic abnormalities, and structural irregularities. The patient then receives hands-on manipulation aimed at addressing any specific dysfunctions, in addition to standard-of-care treatment protocols. Finally, reassessment is performed in order to evaluate the efficacy of intervention.
Literature Review
Our initial inclusion criteria were randomized controlled trials (RCTs) indexed in PubMed studying the efficacy of OMT on adults (> 18 years old) diagnosed with community-acquired pneumonia. We searched PubMed for “osteopath* pneumonia randomized controlled trial”, which yielded a return of six articles. Of these results, three fit the scope of the inclusion criteria.
Because of the limited number of RCTs on the efficacy of OMT in pneumonia patients, we expanded our inclusion criteria to include studies on the efficacy of another manual, non-pharmacologic, adjunctive therapy used in the treatment of pneumonia, namely chest physiotherapy. Chest physiotherapy is defined as a set of techniques designed to improve respiratory efficiency by promoting expansion of the lungs, strengthening respiratory muscles, and eliminating secretions from the lungs16. Chest physiotherapy includes techniques such as percussion and postural drainage along with coughing and deep breathing exercises, which are indicated for the management of pneumonia17. It is clear that the ideal goal of chest physiotherapy is similar to OMT in that both of these manual modalities assist in decreasing the work of breathing and promoting lung expansion. This, it was logical for us to expand our search to include chest physiotherapy.
We then searched PubMed for “physiotherapy pneumonia randomized controlled trial”, which yielded a return of 59 articles. Of these results, three additional studies fit the scope of the inclusion criteria.
When combining the two searches, a total of six RCTs fit our criteria for inclusion. These RCTs are described below, summarized and displayed in Figures 3-4:
The five OMT's described here are a small representation of the osteopathic procedures that can be utilized for a patient with pneumonia when indicated. These techniques focus on improving thoracic cage compliance, improving lymphatic and circulatory flow, and balancing autonomic tone. These techniques are similar to the techniques utilized in the three OMT studies demonstrating efficacy in treating patients with pneumonia.
1. Muscle Energy to Rib 1 - Exhalation Dysfunction 24,25
2. Muscle Energy to Rib 1 - Inhalation Dysfunction 24,25
3. Doming the Thoracic Diaphragm 24,25
4. Seated Rib Raising 24,25
5. Thoracic Pump with Respiratory Assist 24,25
First, Muscle Energy Technique targets the Golgi tendon organs, which are stretch receptors located in skeletal muscle. Upon contraction, Golgi tendon organs are stretched, which activates afferent sensory type Ib nerves transmitting to the spinal cord. In the central nervous system, type Ib nerves synapse upon inhibitory motor neurons, which then provide inhibitory impulses to alpha motor neurons targeting the homonymous muscle group. The end result is relaxation of the initial and synergistic muscles, as well as contraction of antagonistic muscles. This effect is referred to as the Golgi tendon reflex or Inverse Myostatic Reflex. In the application of Muscle Energy Technique to the rib cage, muscles involved in breathing are engaged in isometric resistance. In the case of Rib 1, rib motion can be restricted by pathology related to the scalene muscles. By improving somatic dysfunctions in this respiratory muscle set, Rib 1 moves with greater ease during inspiration and expiration. Treatments that assist thoracic cage motion reduce the impedance of lymphatic flow by respiratory structures, which are located in the thoracic inlet/outlet area. Myofascial restrictions in clavicular region, such as scalene hypertrophy or spasm, can impede the terminal drainage of lymphatic vessels en route to the subclavian veins. Moreover, increased rib cage excursion improves pressure gradients, which further promotes lymph flow.
Second, Doming of the Thoracic Diaphragm Technique involves manipulation of the thoracic diaphragm, which is a principal muscle involved in breathing, blood circulation, lymphatic flow, and other key elements22. This technique involves “doming” the muscle to relieve hypertonicity associated with a flattened or dysfunctional state. Doming refers to the method of applying pressure and stretching the muscle in order to return it to a more normal rounded shape; thus, decreasing it’s hypertonicity. This technique indirectly engages the inferior surface of the diaphragm and increases its excursion during expiration26. Furthermore, the diaphragm assists lymphatic flow by exerting a pump-like propulsion effect on fluid within vessels. Thus, a hindrance in the diaphragm’s physical pumping force will limit lymphatic return to circulation. For instance, a hypertonic diaphragm can hamper the lymphatic flow from the cisterna chili, which is a major vessel that lies behind diaphragmatic attachments. The doming of the thoracic diaphragm technique increases excursion, and consequently there will be both optimal lymph flow and return pressure gradients to normal.
Third, Rib Raising Technique augments lymphatic flow by improving respiratory excursion and reducing sympathetic outflow. Excessive autonomic innervation reduces chest wall mobility by generating hypertonicity of the rib cage musculature and increasing intra-abdominal pressure27. Since lymphatic flow is dependent on pressure gradients generated by adequate respiratory excursion, excessive sympathetic tone can be a hindrance to lymphatic drainage28. Accordingly, this technique addresses this pathology by focusing on sympathetic chain ganglia adjacent to Ribs 2-626. Furthermore, in a study comparing the effect of Rib Raising to a light touch control group, there was a significant decrease in the levels of α-amylase, an established physiological biomarker of sympathetic activity29.
Fourth, Thoracic Pump Technique increases the flow of lymph and other immune cells through a rhythmic, phasic compression of lymphatic vessel walls and regional lymph tissue30, especially the thoracic duct. This technique provides a mechanical force to supplement lymphatic drainage into venous circulation, which is primarily useful in states of obstructed or limited drainage of the extracellular compartment. The oscillatory compressive action produces alternating pressure gradients, which enable lymph to flow through its natural channels in a superior direction.
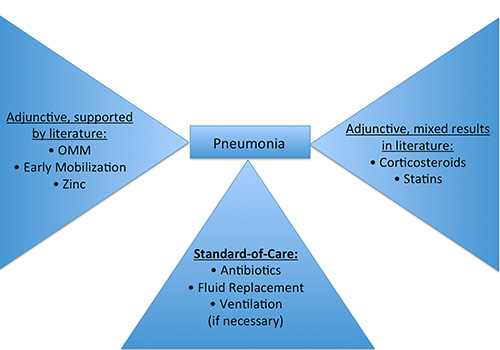
Figure 1. This figure illustrates various components of pneumonia treatment and their efficacy, as supported by current literature4.
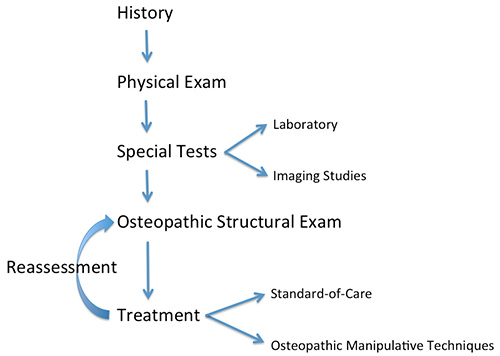
Figure 2. This figure illustrates the step-by-step approach toward patient care utilized by osteopathic physicians.
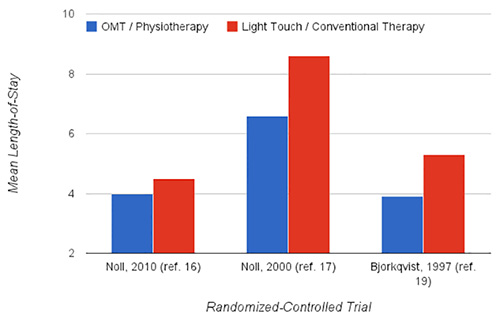
Figure 3. This figure demonstrates significant findings in RCTs comparing length of stay.
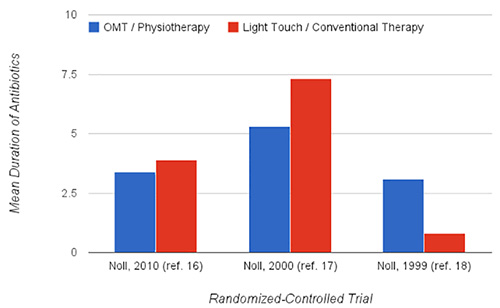
Figure 4. This figure demonstrates significant findings in RCTs comparing duration of antibiotics.
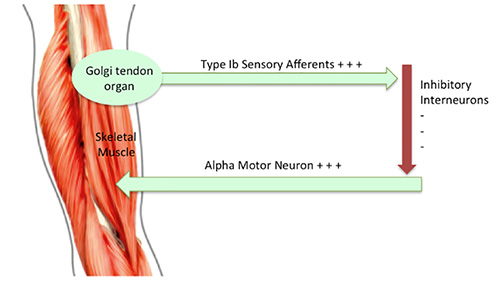
Figure 5. This figure demonstrates the Golgi tendon reflex. When stretched, the Golgi tendon organ is activated and provides feedback to the central nervous system that results in inhibitory impulses being sent to the homonymous muscle.

Figure 6. This figure demonstrates the positional set up for Muscle Energy Technique applied to an exhalation dysfunction of Rib 1.
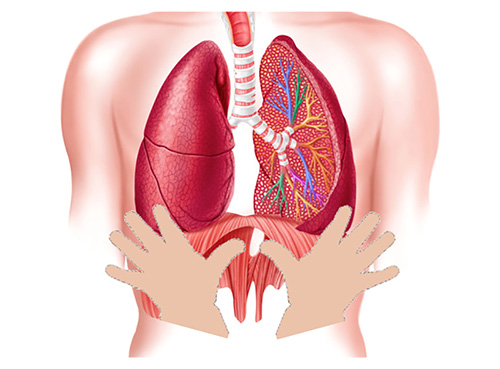
Figure 7. This figure illustrates placement of the thumbs for Doming the Diaphragm Technique, which normalizes the shape of the diaphragm to alleviate abnormal respiratory motions.

Figure 8. This figure demonstrates the positional set up for Doming The Diaphragm technique.
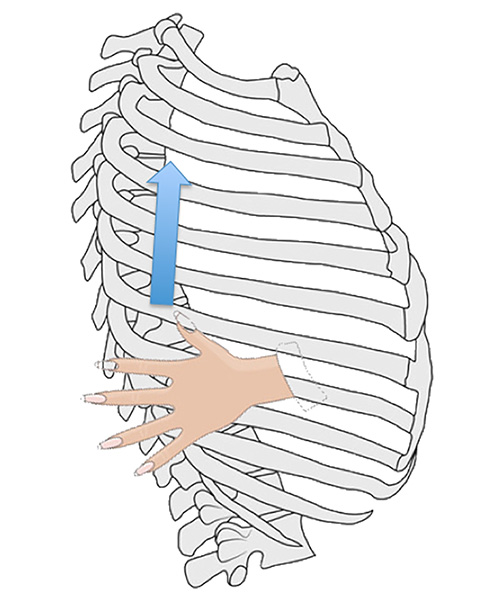
Figure 9. This figure illustrates the Rib Raising Technique, which improves respiratory expansion and alleviates hypertonicity caused by excessive innervation from the sympathetic chain ganglia.

Figure 10. This figure demonstrates the positional set up for Rib Raising Technique.
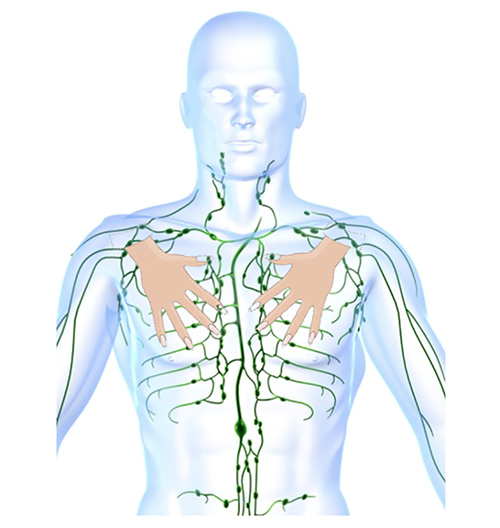
Figure 11. This figure illustrates hand positioning, relative to the lymphatic system, prior to providing downward oscillatory compression in Thoracic Pump Technique.

Figure 12. This figure demonstrates the positional set up for Thoracic Pump Technique.
Osteopathic medicine, when applied to pneumonia patients, aids in restoring health by encouraging normal circulation and immunological function. This is achieved in three sequential steps: removal of dysfunctions obstructing drainage, maximization of respiratory function, and augmentation of flow through lymphoid tissue26. The roles of the lymphatic system include: balancing the composition of interstitial fluid, transportation of excess substances, distribution of immune cells from lymphoid tissues to systemic circulation, and filtration and removal of foreign material from interstitial fluid.
Literature suggests that techniques targeting lymphatic flow are advantageous for treatment of pneumonia by way of altering pressure differentials in the thoracic diaphragm26, improving respiratory function31,32, enhancing antibody response7,33, reducing edema34, activating autonomic-mediated intrinsic lymphatic contractility28, and increasing the abundance of white blood cells in peripheral blood8. Lymphatic pump techniques have been shown to increase cytokines and chemokines in thoracic and intestinal lymph vessels35, while mechanical pressure to certain body regions distant from the location of lymph formation enhances flow into lymphatic systems36. In addition, it has been shown that lymphatic OMT augments leukocyte mobilization and flow in dogs and rats, primarily from gut-associated lymphoid tissue37,38,39,40,41.
Contraindications to performing OMT include osseous fractures, thrombotic events, certain stages of carcinoma, and bacterial infections with a current temperature over 102 degrees Fahrenheit. Osteopathic manual manipulations should only be performed by trained osteopathic physicians. If the physician has difficulty performing the techniques described, we suggest re-positioning and/or further examination of the patient for additional structural abnormalities.
In practice, clinicians may utilize various modifications of the techniques described. For example, a similar version of the rib raising technique can be performed while the patient is supine. In this arrangement, the physician should use the finger-pads of both hands to contact the patient’s rib angles. Utilizing the metacarpophalangeal joints and the treatment table as a fulcrum, the physician should pull laterally by leaning back. This position should be held until a release is felt, then repeat the steps in other areas of the ribs. A modification to the thoracic pump technique involves providing vibratory compressions to the rib cage during patients’ exhalation phase.
In conclusion, we believe that OMT is a valuable adjunctive tool in the treatment of pneumonia. We reviewed established protocols by discussing the steps, mechanisms, and physiologies associated with these therapies. Armed with a better understanding of these techniques, we hope that more physicians will opt to incorporate osteopathic principles into infectious disease protocols.
Martin Gagne was an Associate Editor at the Journal of Visualized Experiments (JoVE) from 2009 to 2011. The remaining authors have no other disclosures.
The authors would like to thank the entire New York Institute of Technology College of Osteopathic Medicine's Department of Osteopathic Manipulative Medicine. This project is funded by the Department of Osteopathic Manipulative Medicine at the New York Institute of Technology College of Osteopathic Medicine.